Neuralgia
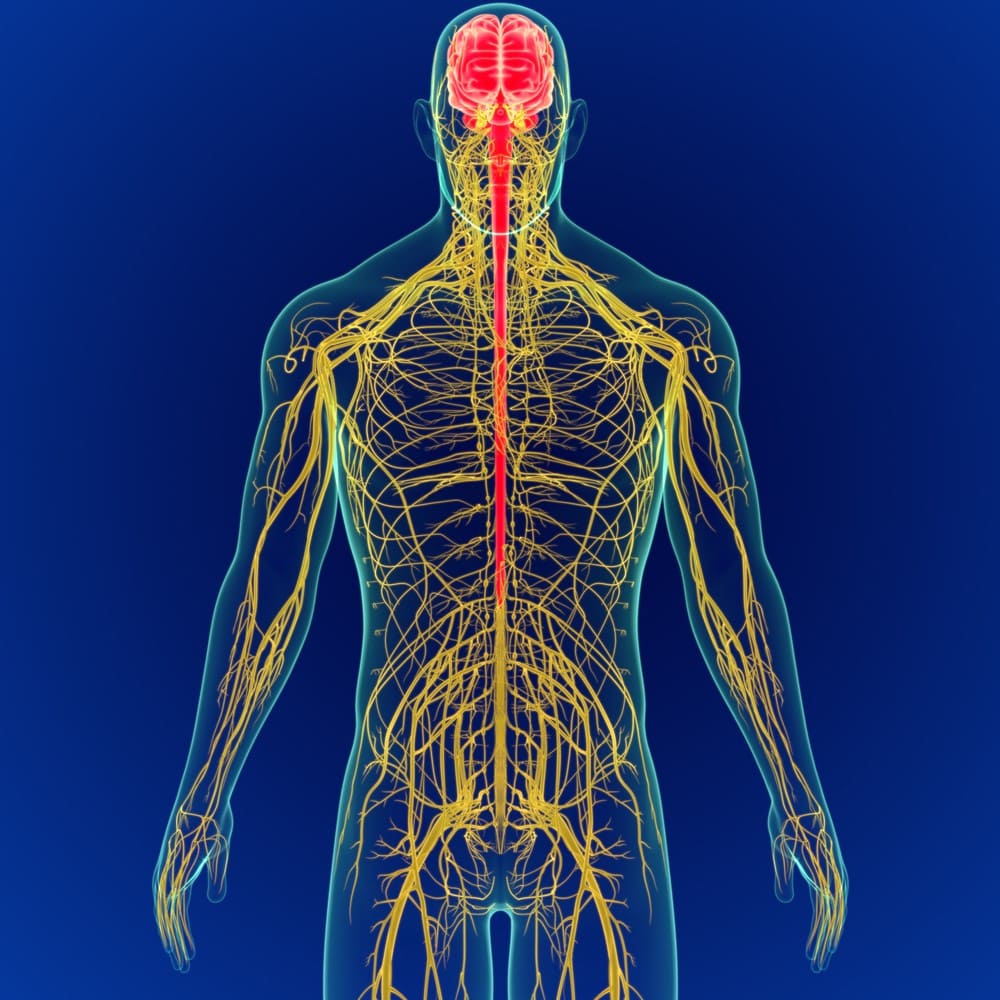
Image source: Shutterstock
Neuralgia is a condition that is caused by different reasons like nerve irritation, nerve damage, nerve infection, etc. It is characterized by sharp and intense pain which follows the pathway of the nerve. Neuralgia may also be called Neuropathic pain or Neurogenic pain. Neuralgia makes it very difficult to carry the basic daily activities. In addition, as the problem is with the nerve, the motor functions are also affected making movements very difficult.
Types of Neuralgia
The pain of Neuralgia come and go, but it generally follows the nerve route. There may be burning or sharp shooting pain across the nerve path. The type and intensity of pain majorly depend on factors like age, current health condition, pain tolerance, comorbidities, etc.
Here are some of the common types of Neuralgia:
A. Trigeminal neuralgia – Trigeminal neuralgia is a chronic condition affecting trigeminal nerve. The disorder can be of two types – typical and atypical. The typical form of trigeminal Neuralgia causes sudden, spasmodic, extreme shock-like facial pain lasting from few seconds to minutes. An atypical form of Trigeminal Neuralgia is characterized by a dull ache, burning sensation, and stabbing pain. Both the types may also exist in the same person.
Image source: Shutterstock
Causes:
i. Trigeminal Neuralgia can be caused by the blood vessels, which may press the nerve when it exits from the brain stem. Regular compression may damage the myelin sheath of the nerve causing symptoms.
ii. Trigeminal Neuralgia may occur in people with conditions like multiple sclerosis (Gass, 1997), leading to the deterioration of the myelin sheath of the Trigeminal nerve.
iii. There can also be trigeminal nerve compression due to tumours (Cirak, 2004) and arteriovenous malformation (García-Pastor, 2006). In rare cases, the trigeminal nerve can get damaged during oral surgery, sinus surgery, facial trauma, and stroke.
B. Sciatic Neuralgia – Sciatic Neuralgia is also called sciatica, which causes numbness and pain in the lower extremities. The condition got its name as the sciatic nerve is involved, which travels from spine to leg. 90% of the cases of sciatica is caused by a herniated disc, which involves nerve root compression. However, lumbar stenoses and tumours are also possible causes of sciatica.
Image source: Shutterstock
The most common symptom of Sciatic Neuralgia is pain which starts from one side of the lower back and moves to the buttocks down to the leg. In rare cases, the back portion of the upper leg is also involved. The pain is at its worst when an individual is sitting or standing for a prolonged duration. In addition, there is numbness, weakness, and tingling of the affected leg, which makes walking and some daily activities difficult.
In sciatica, pain and its associated disability automatically resolve within two weeks. A randomized study compared two NSAIDs with placebo in patients with sciatica and found that 60% of the patients recovered in three months while 70% in 12 months (Weber, 1993). The prognosis of sciatica in most patients is good, but there is also a substantial number of patients who keep on having residual pain for more than one year (Vroomen, 2000).
C. Pudendal Neuralgia – Pudendal Neuralgia is a condition characterized by pain of the pudendal nerve that travels from the anus to the genitals of an individual. The condition is associated with pudendal nerve entrapment (PNE).
The condition is common in women than in men and can be treated using a peripheral nerve block. The common causes of pudendal Neuralgia are:
i. Childbirth (Sultan, 1994)
ii. Surgery (Marcus-Braun, 2012)
iii. Strained bowel movement
iv. Trauma (Heinze, 2012)
v. Pelvic slings
vi. Pelvic floor muscle spasm
vii. Pudendal nerve entrapment or pressure on the pudendal nerve
viii. Bicycle riding (Ramsden, 2003)
Some of the common symptoms of Pudendal Neuralgia are stabbing, burning, or aching pain in the area of the Pudendal nerve, pain while passing urine, painful ejaculations, and genital pain.
D. Occipital Neuralgia – Occipital Neuralgia is a condition that involves occipital nerves. The condition occurs when the nerve is damaged or inflamed. It causes severe shock-like and throbbing pain in the back of the head, upper neck, and behind the ear. Occipital Neuralgia can be caused by injury to the head and/or neck. The pain usually starts from the base of the head and moves to its both the side. The patient may complain of pain behind the eye of the affected side. The pain is described as migraine-like pain by the patient.
It can either be primary or secondary. Secondary occipital Neuralgia is associated with other diseases. There can be various causes of occipital Neuralgia like:
i. Trauma or injury to the occipital nerves.
ii. Compression of the occipital nerves as a result of degenerative cervical spine changes.
iii. Disease of cervical disc.
iv. Diabetes
v. Gout
vi. Tumor of C2 and C3 nerve roots
vii. Infection
viii. Inflammation of blood vessel
ix. Osteoarthritis of the upper cervical spine
E. Glossopharyngeal Neuralgia – Glossopharyngeal Neuralgia is a sharp, shooting pain that an individual experiences in the throat. The pain occurs in the path of the glossopharyngeal nerve located in the neck. The episodes of pain can last for few seconds to few minutes, and it can occur many times throughout the day. Few activities can trigger the painful episodes like:
i. Drinking cold drinks
ii. Sneezing and coughing
iii. Chewing
iv. Swallowing
Individuals suffering from this condition might avoid drinking and eating, as they fear that it can trigger a painful attack. Usually, the condition affects only one side of the head.
There is no apparent cause of Glossopharyngeal Neuralgia, but sometimes when the nerve is irritated due to the compression by the blood vessel around the brainstem, it may cause pain. In rare cases, an elongated styloid process can also cause pain. The condition is called Eagle syndrome. Any trauma due to surgical procedure may also result in glossopharyngeal Neuralgia. Other causes of glossopharyngeal Neuralgia include tumours, infections, and vascular abnormalities. The symptoms of glossopharyngeal Neuralgia are also common in patients with multiple sclerosis.
F. Postherpetic Neuralgia – Postherpetic Neuralgia is the complication of shingles that affects the skin, giving rise to burning pain even when the rash of the shingles has disappeared. The risk of Neuralgia is high in older people, and there is no cure for the same. In most cases, the symptoms improve with time.
Symptoms are most commonly limited to the area where rashes of the shingles first appeared, which is mainly around your trunk. Signs and symptoms include pain that lasts for longer than three months after the shingles rash has disappeared, along with the sensitivity to light touch. In rare cases, postherpetic Neuralgia can also cause numbness and itch.
Importance of physiotherapy in Neuralgia
One of the most important aspects of treatment in Neuralgia is pain management. Pain is the most disabling symptom in patients with Neuralgia. Physiotherapy can be very helpful in pain management.
Physiotherapy treatment of Neuralgia includes:
1. Identifying the triggers and treating them.
2. Easing the pain and manage the other symptoms associated with Neuralgia.
Various physiotherapy techniques are used to reduce the pain in Neuralgia like:
a. Cryotherapy – It is one of the most commonly used techniques to reduce pain. Using cold packs to block the sensation of the pain is the best way to manage the symptoms of Neuralgia. Cryotherapy can be both normal with ice packs or gravity assisted or compression based etc.,
Image source: Shutterstock
b. Massage therapy – Massage therapy is used to relieve the pain in occipital Neuralgia, where the patient mainly complains of stabbing headaches. A good massage on the painful area can improve the nerve’s blood and oxygen flow, which can help heal the damaged nerves.
c. Transcutaneous electrical nerve stimulation (TENS) – TENS therapy improves the pain in the patient with Neuralgia by blocking the pain signals (Gibson, 2017).
In addition to pain control, a physiotherapist will also incorporate muscle strengthening, flexibility exercises (ePainAssist, 2019), and aerobic exercises to improve the symptoms of Neuralgia.
Unfortunately, treating Neuralgia is not an easy task. It needs a proper assessment to identify the cause, severity, and location of your pain. Other treatment options for Neuralgia are surgery, nerve ablation, nerve block, and anesthetic shots.
Visit Progressive Care to find out the best-suited treatment option for Neuralgia.
References:
1. Gass, A. (1997, October). Trigeminal Neuralgia in patients with multiple sclerosis: lesion localization with magnetic resonance imaging. PubMed. https://pubmed.ncbi.nlm.nih.gov/9339705/
2. Cirak, B. (2004, January). Trigeminal Neuralgia caused by intracranial epidermoid tumor: report of a case and review the different therapeutic modalities. PubMed. https://pubmed.ncbi.nlm.nih.gov/16868626/
3. García-Pastor, C. (2006, August). Trigeminal Neuralgia was secondary to arteriovenous malformations of the posterior fossa. PubMed. https://pubmed.ncbi.nlm.nih.gov/16876635/
4. Weber, H. (1993, September 1). The natural course of acute sciatica with nerve root symptoms in a double-blind placebo-controlled trial evaluating the effect of piroxicam. PubMed. https://pubmed.ncbi.nlm.nih.gov/8235813/
5. Vroomen, P. C. (2000, December). Conservative treatment of sciatica: a systematic review. PubMed. https://pubmed.ncbi.nlm.nih.gov/11132976/
6. Sultan, A. H. (1994, January). Pudendal nerve damage during labour: prospective study before and after childbirth. PubMed. https://pubmed.ncbi.nlm.nih.gov/8297863/
7. Marcus-Braun, N. (2012, June). Persistent pelvic pain following transvaginal mesh surgery: a cause for mesh removal. PubMed. https://pubmed.ncbi.nlm.nih.gov/22464208/
8. Heinze, K. (2012, August). [Neuralgia of the pudendal nerve following violent trauma: analgesia by pudendal neuromodulation]. PubMed. https://pubmed.ncbi.nlm.nih.gov/22751935/
9. Ramsden, C. E. (2003, June). Pudendal nerve entrapment is a source of intractable perineal pain. PubMed. https://pubmed.ncbi.nlm.nih.gov/12820792/
10. Gibson, W. (2017, September 14). Transcutaneous electrical nerve stimulation (TENS) for neuropathic pain in adults. PubMed. https://pubmed.ncbi.nlm.nih.gov/28905362/
11. ePainAssist, T. (2019, July 15). Best Exercises/Activities For Trigeminal Neuralgia Patients. EPainAssist. https://www.epainassist.com/fitness-and-exercise/best-exercises-activities-for-trigeminal-neuralgia-patients
For more details contact
us on 📞9618906780
